Hyperglycemia resolved Uremia Sepsis -blood cells contain kleibsiella species Hypoalbuminemia ?Nutritional UTI, AKI, denovo DM2,NC/NC Anemia Bed sores(+)Alcohol dependence andTobacco dependence
DR.ROSHINI REDDY
August 11, 2021
Greetings to one and all who are currently reading my blog.
This is an online E - log book to discuss our patients de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online portfolio and your valuable inputs on the comment box.
Note: This is an ongoing case and will be uploaded as and when information is provided. This E-Log has been made under the guidance of DR.ZAIN ALAM.
Case scenario:-
75 yr old male, farmer by occupation, came to the casuality with-
CHIEF COMPLAINTS:-
Fever since 10days
Altered sensorium since 6pm on the day of admission
HISTORY OF PAST ILLNESS:-
Patient was apparently asymptomatic until 12months back when they observed patient having decreased interest in doing work and felt tired throught the day.But the patient was able to move with walking stand and meet relatives and used to ask for food and alcohol .
OD denies any episodes of cryingspells, low mood, suicidability, loss of appetite, during this period.
H/o fall from cycle ? 6ys back decreased alcohol and suffered from fracture of hip(femur neck ) right side didn't visit hospital had local treatment since then staying at home and stopped field work.
Patient was able to do his daily activities can also used to ride cycle occasionally.
From 1 yr patient became more lethargic, Not interacting actively with the family members, spending more time on bed.
Bed Sores Over B/L back part of the legs
10 days back patient developed fever with tremors in hands and jaws and muttering of words due to pain with decreased interaction. Since 2days with ulcers on back so, they took him to local hospital and was treated later patient felt better, able to speak properly and ate food.
After 4 days patient has similar episodes with fever and was brought to here to hospital.
H/o Alcohol use since 30yrs, decreased consumption since 2 months, 90ml (-3 units) per week.
Tobacco use since 30yrs( consumes 10-15 beedis per day)
H/o disinhibited behaviour since 2 months.
No h/o self talking, self laughing, suspicious memory disturbances, irritability, repetitve thoughts.
PAST HISTORY:-
N/K/C DIABETES, HYPERTENSION, ASTHMA, TB, EPILEPSY.
No H/O any surgeries in the past.
FAMILY HISTORY:-
Not significant
PERSONAL HISTORY:-
Diet-Mixed
Appetite-normal
Bowel and bladder movements- Regular
Sleep- Adequate
GENERAL EXAMINATION:-
Patient is conscious and co operative,
Drowsy but arousable
Oriented to person,
place -,
time -,
Registration -,
attention -,
Recall -
Moderately built and moderately nourished.
Consent obtained
On examination:
No pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
No edema.
Vitals:-
Temp- afebrile.
PR:96 BPM.
RR: 16 CPM.
Bp: 80/60 mm Hg
Spo2 : 98%
GRBS 196 MG%.
SYSTEMIC EXAMINATION:-
A. Cardiovascular system
S1 S2 HEARD
NO MURMURS.
B. Respiratory system
NVBS heard
BAE +
TRACHEA CENTRAL.
C. Per abdominal examination
SOFT
NON TENDER
NON DISTENDED.
D.CNS EXAMINATION:-
1. Higher Mental Function:-
Drowsy but arousable
Oriented to person, place -, time -, Registration -, attention -, Recall -
Language - spontaneous speech , - fluency, - comprehension
2. Cranial nerves - all cranial nerves
- gag reflex
- vulva position
3. Motor system - attitude -
Rt. Lt.
Tone. UL. - -
LL. hypo. -
Power. UL. - -
LL. - -
Reflexes. B + +
T. - -
S. - -
K. - -
A. - -
Plantars
4. Sensory system - Couldn't be done
Deep pain +
Superficial pain +
5. Cerebellar system - couldn't be done
6. No signs of meningial irritation/ meningitis
OD denies any psychiatric illness in family.
Motor System Examination :- Patient is lying on bed in upright position
Eye To Eye Examination - ,
BILATERAL swelling of arms
Psycho Motor Activity:-DECREASED
Rapport established with difficulty
Speech
Tone, Volume and Rate- DECREASED,
Reaction Time INCREASED.
--able to answer on repeated questioning by relatives
--mood and other Mental status examination-could not be established.
BEDSORES
INVESTIGATIONS:-
12/08/21
Hemogram report
Ultrasound report
HIV 1/2 rapid test
Anti HCV antibodies
RFT
RTPCR
ESR
Urine test for ketone bodies
Complete urine examination
Liver function test
2D Echo report
No Rwma ,No ms /as
Mild Lvh + sclerotic av
Mild mr+ trivial ar+
Diastolic dysfunction +
IVC dialated (1.45cms) normal
No pe/lv clot
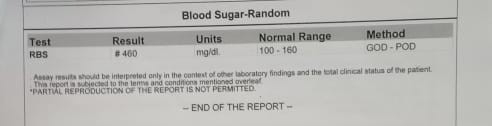
Random blood sugar
ABG Report
X Ray
13/08/21
RFT
Hemogram report
X ray
14/8/21
PSYCHIATRIC CROSS CONSULTATION:-
This is the case of 75yr old male diagnosed ?hyperglycemia, hypoalbuminenia, UTI, AKI,denovo DM2, With anemia and bed sores reffered i/v/o chronic illness which could be psychiatric manifestation as patient c/o of pain and experiencing distress on evaluation.
-- History noted from OD(objective data)
--Patient is lying on bed with Ryles tube and IV cannuli responding with only monosyllable on commands
--Unable to move both Upper Limbs and Lower limbs
OD denies any psychiatric illness in family.
Motor System Examination :- Patient is lying on bed in upright position
Eye To Eye Examination - ,
BILATERAL swelling of arms
Psycho Motor Activity:-DECREASED
Rapport established with difficulty
Speech
Tone, Volume and Rate- DECREASED,
Reaction Time INCREASED.
--able to answer on repeated questioning by relatives
--mood and other Mental status examination-
--IMPRESSION- adjustment issue secondary Alcohol dependence currently abstinent due to illness
*Tobacco dependence currently ? withdrawal
Rx-
patient attenders councelled
T.SERTA 25 mg OD every morning
LOSENGES 2mg sos
PROVISINAL DIAGNOSIS:-
Fever under evaluation
Altered sensorium
Hyperglycemia
TREATMENT:-
Day-1
INJ HAI IV ( 39ml NS + HAI)@ 6ml/hr followed by infusion according to Alog-1
1 hrly GRBS
INJ PIPTAZ 4.5gm IV stat followed by INJ PIPTAZ 2.25gm I've stat
INJ OPTINEURON 1 Amo in 100ml NS/IV/OD
Protein powder -2tsp in 1 glass of milk /twice a day in rules tube
Patient feeds milk with protein powder - 100 my every 2 ND hrly and plain water every hrly.
Hrly GRBS charting
INJ NORADRENALINE( 2amp in 50ml NS) @2ml /hr to maintain MAP >or = 6
Day -2
1.IVF 10NS @75 ml/hr
2.INJ PIPITAZ 2.25gm/IV/TID
3.INJ OPTINEURON 1amp in 100ml NS
4.TAB OROFER -XT/PO/OD
5.TAB LASIX 20mg/PO/OD
6.Protein -x-powder -2tsp in 1 glass of milk /Rt feeds 2nd hrly
Rt-plain water - 200ml /hrly
7.INJ HALI /SC/TID
8.PR/BP/RR/SpO2 charting 2nd hourly
9. GRBS charting 6th hourly
10. Inj TRAMADOL 1 amp in 100 ml NS IV/OD
11.TAB VITRACET 1/2 tab/RT
Day -3
- 1. IVF NS @ 75ml/hr
- 2. Inj PIPTAZ 2.25gm/IV/TID
- 3. Inj Optineuron 1 amp in 100ml NS IV/OD
- 4. Tab Orofer - XT/RT/OD
- 5. Tab Lasix 20mg/RT/OD(if SBP > 100 mg 8am---- x ---- x
- 6. Protein-X powder 2tsp in 1 glass of milk/ RT feed 2nd hourly
- 7. Inj HAI/SC/TID after informing Sugars to ICU Ph
- 8. Inj Tramadol 1 amp in 100 ml NS/IV/OD
- 9. Tab Ultracet 1/2 tablet/RT/QID1/2----1/2----1/2----1/2
- 10. Two egg whites/day
- 11. Bp/PR/RR/SPO2 Charting 2nd hourly
- 12. GRBS Charting 6th hourly 8am----2pm----8pm----2am
Day -4-
- IVF 10 NS @75 ml/hr
- Inj.Piptaj 2.25 gm/IV/T
- Inj.Opti Neuron 1 amp in 100ml NS/N/OD
- TAB.Fluconazole 150 mg/PO/OD
- TAB. OROFER RT/OD
- TAB.Lasix 20 mg/RT/OD
- Protein-x powder 2 tbsp in 1 glass of milk,RT feed 2 nd hourly RT plain water-200 ml hourly
- Inj.HAI /SC/TID
- Inj.TRAMADOL lamp in 100 pal NS/IV/OD
- TAB.ULTRACET 1/2 tab/RT/OD
- 2 egg whites/day
- BP/PR/RR/Spo2 charting 2nd hourly
- GRBS charting 6th hourly 8 AM-2 PM-8 PM-2 AM
DAY-5
IVF 10NS @75ml/hrly
INJ PIPTAZ 2.25 gm IV/TID
INJ OPTINEURON 1amp in 100 ml NS/ IV /OD
TAB FLUCONAZOLE 150mg PO/OD
TAB OROFER (5) RT/OD
TAB LASIX 20mg RT /OD
Protein-x powder 2 tbsp in 1 glass of milk
TAB GLICIAZIDE PO/OD (1/2 tab)
I/O CHARTING
DISCHARGE SUMMARY
Case:-
75 yr old male came to the casuality with c/o fever since 10 days,Altered sensorium since 6:00pm.
CHIEF COMPLAINTS:-Fever since 10days,Altered sensorium since 6pm.
HISTORY OF PRESENT ILLNESS:-
Patient was apparently alright till 10 days back then he had fever insidious onset, low grade Continous, Relieved on taking medication, Not associated with chills and Rigors.
Today morning patient was talking normally from 6 pm.patient was just muttering words.
HISTORY OF PAST ILLNESS:-
Patient was farmer by occupation; one day 6 yrs back patient drank Alcohol, fell from cycle, got fractured in the Right femur neck fracture got treated from local RMP.lethargic, Not interacting actively with the family members, spending more time on bed.
Bed Sores Over B/L back part of the legs
PAST HISTORY:-
No h/o similar complaints before.
No known comorbidities.
GENERAL EXAMINATION:-
No pallor,No icterus,No cyanosis,No clubbing
No lymphadenopathy,No edema.
Vitals:-
Temp- afebrile.
PR:96 BPM.
RR: 16 CPM.
Bp: 80/60 mm Hg
Spo2 : 98%
GRBS 196 MG%.
SYSTEMIC EXAMINATION:-
A. Cardiovascular system
S1 S2 HEARD,NO MURMURS.
B. Respiratory system
NVBS heard,BAE +,TRACHEA CENTRAL.
C. Per abdominal examination
SOFT,NON TENDER,NON DISTENDED.
D. Central nervous system
CONSCIOUS,NO SIGNS OF MENINGEAL IRRITATION.
**Reflexes:-
RT. LT.
BICEPS. + +
TRICEPS. + +
SUPINATOR. + +
KNEE. + +
ANKLE. + +
PLANTAR: FLEXOR.
PROVISINAL DIAGNOSIS:-
Fever under evaluation
Altered sensorium
Hyperglycemia
SOAP NOTES
Day -1
Subjective-
C/oFever
C/o altered sensorium
Objective:-
Temperature
At 4am 98 F
At 8am 37.5 C
BP 80/60 mmHg
PR 96/mins
RR: 16 CPM.
Assessment :-
Hyperglycemia
Fever under evaluation
Altered sensorium
Plan of care:-
1.INJ HAI IV ( 39ml NS + HAI)@ 6ml/hr followed by infusion according to Alog-1
1 hrly GRBS
2.INJ PIPTAZ 4.5gm IV stat followed by INJ PIPTAZ 2.25gm I've stat
3.INJ OPTINEURON 1 Amo in 100ml NS/IV/OD
4.Protein powder -2tsp in 1 glass of milk /twice a day
5.Patient feeds milk with protein powder - 100 my every 2 ND hrly and plain water every hrly.
6.Hrly GRBS charting
7.INJ NORADRENALINE( 2amp in 50ml NS) @2ml /hr to maintain MAP >or = 6
Day-2
Subjective:-
C/o fever
C/o altered sensorium
Objective:-
Temparature-
At 4am -38 C
At 8am -37.5 C
BP-80/50
PR-96/min
RR-21 cpm
Assessment :-
Hyperglycemia resolved
Right lobe pneumonia
Hypoalbuminemia ?Nutritional
UTI, AKI, denovo DM2,
NC/NC Anemia
Bed sores
Plan of care:-
1.IVF 10NS @75 ml/hr
2.INJ PIPITAZ 2.25gm/IV/TID
3.INJ OPTINEURON 1amp in 100ml NS
4.TAB OROFER -XT/PO/OD
5.TAB LASIX 20mg/PO/OD
6.Protein -x-powder -2tsp in 1 glass of milk /Rt feeds 2nd hrly
Rt-plain water - 200ml /hrly
7.INJ HALI /SC/TID
8.PR/BP/RR/SpO2 charting 2nd hourly
9. GRBS charting 6th hourly
10. Inj TRAMADOL 1 amp in 100 ml NS IV/OD
11.TAB VITRACET 1/2 tab/RT
SOAP NOTES Day-3
Subjective:-
C/o fever
c/o altered sensorium
Objective :-
Tempature-
4-12 am -37.5 C
4-8pm-98.5 F
12pm-37.5 C
BP 110/70mmHg
PR 92 bpm
Assessment:-
Hyperglycemia resolved
Shorts not paused
Plan of care:-
1. IVF NS @ 75ml/hr
2. Inj PIPTAZ 2.25gm/IV/TID
3. Inj Optineuron 1 amp in 100ml NS IV/OD
4. Tab Orofer - XT/RT/OD
5. Tab Lasix 20mg/RT/OD(if SBP > 100 mg 8am---- x ---- x
6. Protein-X powder 2tsp in 1 glass of milk/ RT feed 2nd hourly
7. Inj HAI/SC/TID after informing Sugars to ICU Ph
8. Inj Tramadol 1 amp in 100 ml NS/IV/OD
9. Tab Ultracet 1/2 tablet/RT/QID1/2----1/2----1/2----1/2
10. Two egg whites/day
11. Bp/PR/RR/SPO2 Charting 2nd hourly
12. GRBS Charting 6th hourly 8am----2pm----8pm----2am
SOAP NOTES-Day-4
Subjective:-
c/o fever and altered sensorium
Objective :-
Temperature-
4-8am 37.5 C
8-12am- 98.5-99 F
BP 100/70mmHg
PR 84bpm
Assessment:-
Hyperglycemia resolved
Back pain
Plan of care:-
Rx:
IVF 10 NS @75 ml/hr
Inj.Piptaj 2.25 gm/IV/T
Inj.Opti Neuron 1 amp in 100ml NS/N/OD
TAB.Fluconazole 150 mg/PO/OD
TAB. OROFER RT/OD
TAB.Lasix 20 mg/RT/OD
Protein-x powder 2 tbsp in 1 glass of milk,RT feed 2 nd hourly RT plain water-200 ml hourly
Inj.HAI /SC/TID
Inj.TRAMADOL lamp in 100 pal NS/IV/OD
TAB.ULTRACET 1/2 tab/RT/OD
2 egg whites/day
BP/PR/RR/Spo2 charting 2nd hourly
GRBS charting 6th hourly 8 AM-2 PM-8 PM-2 AM
Soap notes day-5
Subjective :-
C/o fever and altered sensorium
Objective:-
Temperature-
4-8am-37.5 C
BP-100/70 mmHg
PR-81bpm
Assessment:-
Hyperglycemia resolved
Uremia
Sepsis -blood cells contain kleibsiella species
Hypoalbuminemia ?Nutritional
UTI, AKI, denovo DM2,
NC/NC Anemia
Bed sores(+)
Alcohol dependence and
Tobacco dependence
Plan of care:-
IVF 10NS @75ml/hrly
INJ PIPTAZ 2.25 gm IV/TID
INJ OPTINEURON 1amp in 100 ml NS/ IV /OD
TAB FLUCONAZOLE 150mg PO/OD
TAB OROFER (5) RT/OD
TAB LASIX 20mg RT /OD
Protein-x powder 2 tbsp in 1 glass of milk
TAB GLICIAZIDE PO/OD (1/2 tab)
I/O CHARTING


























Comments
Post a Comment